Wilderness First Aid
The Framework
The framework includes checking for scene safety, the primary and secondary surveys, and the ever-important SOAP note. This is the routine that you do with every patient every time so that you don’t forget anything important.
- STOP…think…Scene Safety and Body Substance Isolation (i.e. gloves)…Is it safe for:
- You?
- Your Co and FOPpers?
- Your patient? This is where you and your co split up the group and medical responsibilities.
- STOP…think…What was the MOI? Do you need to stabilize the patient’s head? Communicate with the injured person and tell them to lie still; keep talking to reassure them. Approach carefully.
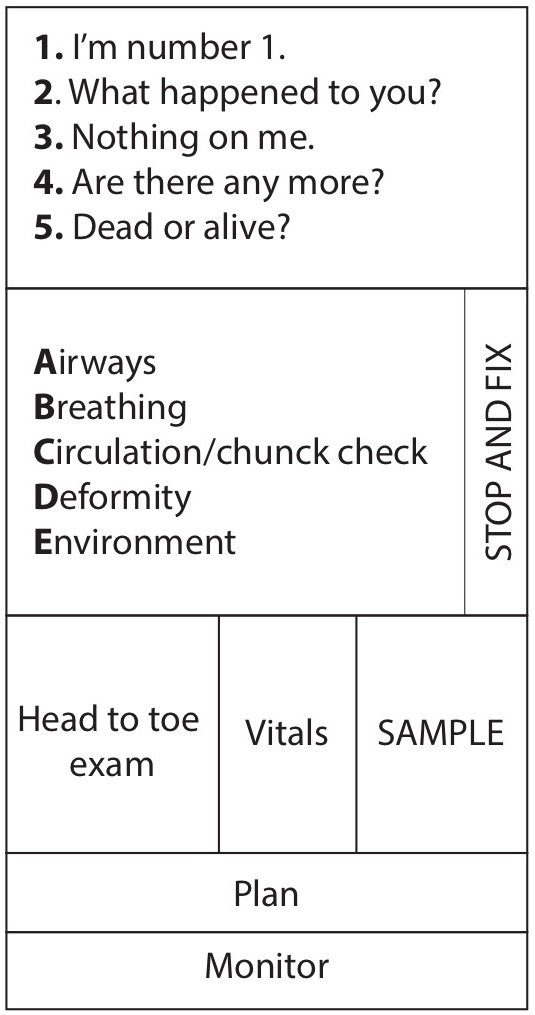
Primary Survey
The purpose is to get a primary history (what happened?), find any life-threatening injuries and treat them, and prevent further life-threatening injuries.
Look, listen, and feel for ABCs - the brain can only survive for six minutes without oxygen!
- Airway: Look for any obstructions, listen for fluid or gurgling, feel for air moving in and out of airway. Remove obstructions before proceeding.
- Breathing: Look to see if chest wall is moving properly, listen for wheezing or unusual sounds, feel for movement of air. Do artificial respiration if not breathing.
- Circulation: Look for severe bleeding (remember to look for bleeding of torso, and for femur fractures), listen for heartbeat, feel for pulse at neck and wrist. If there is no pulse, do CPR. If there is severe bleeding, control it with direct pressure.
Next:
- Disability/Deformity: Protect the head and back and check sensation in extremities for a spinal MOI. Do a chunk check to find obvious deformities or injuries.
- Environment: Is it warm, cold, wet, dry? If so, fix it!
STOP…think…RELAX. If you have completed the primary survey, your patient is just fine at the moment. It is more important to calmly gather information and to begin preparing a comprehensive SOAP note and possible evacuation plan (if necessary) than to rush through the survey and stress yourself, your co, and your FOPpers out while missing bits of information.
Secondary Survey
The purpose is to get a more detailed history, establish the severity of injuries (take vital signs every 5-15 minutes), locate all injuries, know the overall medical condition of patient (AMPLE history), and record the patient’s condition (SOAP note). Start with the element most relevant to your patient. For example, with a trauma patient you would probably start with the patient exam, whereas with a patient with an illness you might start with the history.
Remember to fill out the SOAP note with this info. The SOAP note is a legal document. You must write one if you are going to evacuate, and it’s not a bad idea to start one if you have any inkling that an evacuation will be necessary.
Vital Signs
- Level of Consciousness (LOC)/AVPU Scale
- Alert? How alert and oriented? A&O x 1 = person (they only know who they are). A&O x 2 = place (they also know their location). A&O x 3 = time (they know the time & date).
- Verbally responsive? They’re unconscious, but do they respond to sound? See if they move or attempt to speak when addressed; see if they can follow a request to blink or move a limb.
- Painfully responsive? Do they groan or move in response to a knuckle rubbed on the sternum?
- Unresponsive? No response to verbal or painful stimuli. Comatose.
- Respiratory Rate & Effort
- Respiratory Rate: Check by counting the number of breaths per minute. 10-20 breaths per minute are normal.
- Respiratory Effort: Are they having to work hard to breathe? Ask if they feel short of breath.
- Heart Rate & Quality
- Heart Rate: Check pulse. Normal = 50-100 beats per minute.
- Quality: How does the pulse feel? Strong? Thready? Irregular?
- Skin
- Color: Is there a perfusion of blood to the skin? Because skin color varies, look at non-pigmented areas of the body: nail beds, under eyelids, in mouth.
- Temperature: Are they hot or cold to the touch? Check abdomen and armpit.
- Moisture: Are they dry, wet, or sweaty?
- Other Vital Signs (WFR level and above)
- Pupils (PERRL): Equal, round, and reactive to light?
- Blood Pressure: Use pulses in the extremities to estimate BP when lacking a BP cuff.
Patient Exam
Head-to-toe inspection. Check head, neck, chest, abdomen, legs, arms, and then back. Be sure to look at any area that elicits a response. Apply firm pressure.
Be sure to check CSMs in extremities:
- Circulation (check for all pulses)
- Sensation (feeling in all extremities)
- Movement (ask them to move extremities).
AMPLE History
- Allergies: Allergic to foods, medications, insects etc.? Severity and treatment?
- Medications: Taking any current medications (prescriptions or over-the-counter)? How often and how much? Dose taken today?
- Past Pertinent History: Is there any past injury or illness that might contribute to the current problem?
- Last Ins and Outs: Last time they ate or drank (and what they ate/drank), last urination or bowel movement?
- Events Leading up to the Problem: What happened just before the accident?
STOP…think…Monitor patient and plan for the evacuation if necessary. Keep recording vitals, etc., in the SOAP note.
Management of Spinal Injuries & Clearing the Spine
MOI for spinal cord injuries:
- Falls, especially with high speed, tumbling, or any fall from 3X body height or more
- Impact (combination of impact and rapid deceleration, such as in an auto accident)
- Any head injury resulting in loss of consciousness
- Diving injury
- Direct blows to head, neck, or spine
Symptoms of a spinal injury:
- MOI for a spinal injury
- Pain: radiating, diffuse, pain with motion, or points tender upon palpation
- Loss of consciousness
- Guarding or spasming of muscles (ex “stiff” neck)
- Paresthesia (pins and needles sensation)
- Numbness
- Paralysis
- Locked sensation
- Deformity
To treat, bring the patient to position of function (“decrumple”) and immobilize them.
In order to “clear” the spine, you must have (in this order):
- Patient Reliability: Patient is A&O x 3, not influenced by alcohol, drugs, or cold/ heat.
- No Distracting Pain: If there is a distracting injury, your treatment must have reduced the pain to a point where the patient can reliably report any symptoms of a spinal injury.
- No signs or symptoms, based on reassessments over time: there is no pain in the entire length of the back, no radiating pain, or numbness. A patient with only an MOI and no other symptoms may be cleared to walk out.
- Range of Motion Test: This is the final step, taken only if conditions 1, 2, and 3 are met. The rescuer supports but does not move the patient through the ROM test. Any pain, stiffness, or locked sensation requires full immobilization.
To conduct a range of motion test:
- First rotate head slowly to one side, then the other.
- Second, hyper-extend the head: slowly look up.
- Third, flex the neck by slowly looking down. (It’s important that this comes last, since this movement could aggravate a spinal injury.)
Shock
Shock occurs when the blood can no longer bring enough oxygen to vital organs. There are several types of shock:
- Hypovolemic Shock: Decreasing blood volume due to blood loss or dehydration.
- Cardiogenic Shock: Decreasing blood flow when heart stops working as in the case of a heart attack (lightening causes this).
- Neurogenic Shock: Loss of vascular tone resulting in increased vascular space/expanding arteries (i.e., a head/spinal injury or severe infection).
Signs and symptoms:
- LOC: Restless, anxious, confused or vacant
- RR: Rapid and shallow
- HR: Rapid, weak, thready
- SKIN: pale, cool, clammy
- Patient may collapse, be nauseous, or vomit
[WFR topic: Decompensatory shock occurs when the body’s attempt to compensate by raising HR and RR are not sufficient to maintain circulation. Decompensatory shock is evidenced by falling BP.]
Care:
- Treat the cause!!!
- Maintain an open airway.
- Keep the patient lying prone with legs elevated.
- Monitor vital signs.
Soft Tissue Injuries
Soft tissues are everything but the bones; common soft tissue injuries affect the skin and structures immediately under the skin (fat, muscles, and blood vessels).
Wounds
- BSI!
- To control heavy bleeding: Apply direct pressure for about 10 minutes, elevate the wound and bandage it (don’t remove the bandage, just keep adding them). If direct pressure and elevation do not lessen the blood flow, remove the dressings and apply digital pressure (with a gloved hand) to the cut artery.
- Clean with pressurized water through hole in bag, using cleanest water available.
- Bandage, and keep cleaning and re-cleaning and monitor for signs of infection. Change bandages every 24 hours (sooner if conditions are dirty or wet).
- An antibiotic can be applied to abrasions after cleaning and before bandaging, but don’t fill a laceration or puncture wound with ointment as it will seal bacteria inside.
- A patient should be evacuated for stitches if:
- The laceration is longer than 1/2 inches, if the cut is deep, and/or if scarring is a concern
- If the edges of skin do not fall together (i.e. flesh is exposed beneath)
- If the cut is on face, hands, or over a joint
- [WFR topic: If there is an injury to a blood vessel, ligament, or tendon]
Blisters
The key is to stop it at a hot spot! Treat popped blisters as a wound; un-popped ones can by padded with an ring of moleskin (in multiple layers for large blisters) to prevent them from popping.
Burns
Stop the burning by removing the source and immediately immersing the burned area in a lot of cold water. Assess the severity of the burn. Apply a moist bandage that is as sterile as possible. Then apply an occlusive layer to keep moisture in. Burned areas will lose moisture, so watch for dehydration.
Signs of Infection
Swelling, redness, and heat in the affected area; pain and pus formation. Infection is worsening if red streaks proceed from the infected area to the lymphatic ducts (swollen lymph nodes will indicated this, too). Fever and chills will occur if infection has spread systemically - at this stage, it’s highly dangerous.
Musculoskeletal Injuries
Musculoskeletal injuries are injuries to bones and joints.
Dislocations
- Pulling apart of a joint; may injure muscles, tendons, ligaments, and cartilage. May be associated with a fracture. Sometimes a dislocation will go back in immediately, but if they stay dislocated, it’s extremely painful and the reduced circulation can put future function of the limb at risk.
- Symptoms: Diffuse pain, reduced range of movement, reduced CSMs, deformity.
- Care:
- Shoulder Dislocation: position patient face down on sturdy surface high enough for injured arm to hang down and attach a 5- to 10-pound weight (water bottle works well) to wrist. The goal is to exhaust the muscles, so the shoulder will reduce, but this might take hours.
- Evacuate for all dislocations (there isn’t much you can do with WFA certification for dislocations)
- [WFR topic: Pull traction in-line to reduce the dislocation, then immobilize the area by splinting. (RICE as appropriate.) Use a steady, firm pull and have someone provide counter-traction; use slow, gentle movements to gradually realign the joint.]
Sprains and Strains
- Over-stretching of a joint.
- Symptoms: Generalized pain around a joint, pain with movement of joint, minimal pain with weight-bearing, possible dramatic swelling, discoloration over time.
- Treat by RICE (Rest, Ice, Compression, Elevation).
Fractures
- Breaking of bones.
- Symptoms: Lack of normal movement or function for affected area, visible deformity, sound of “snap” or “pop” at the time of the injury, discoloration and swelling, point tenderness, crepitation (sound of grinding).
- Treat by splinting. The goal is to stabilize the joints above and below for a bone injury, or to stabilize the bones above and below for a joint injury. A good splint should be rigid, well padded, well compressed and durable. Keep checking CSMs (circulation sensation and motor function in distal extremity).
- [WFR topic: In the case of a femur fracture (one on the shaft, not at the hip or knee), a traction splint should be used to prevent damage to the femoral artery. Symptoms of such a fracture: severe pain and muscle spasms in the upper leg and upon palpation; possible angulation, discoloration, or exposed bone ends.
- Pull manual traction at ankle, in-line.
- Cut away clothing.
- Traction splint: Use a stick or hiking pole at least a foot longer than the leg. Hitch at the ankle and at the hip with cravats or p-cord; replace manual traction with mechanical traction using trucker’s hitch. Stabilize by tying legs together.]
- Try to ascertain whether any blood vessels were harmed by the broken bone.
Environmental Concerns
Hypothermia
- Hypothermia is the lowering of the body’s core temperature to a level where normal brain and muscle function are impaired.
- Signs/symptoms: Loss of fine motor skills, confusion, shivering. People suffering from hypothermia will often deny that anything is wrong.
- Treatment: Prevention is key: wear raingear to avoid getting wet, eat snacks often, stay hydrated. Care: Get the patient dry, moving, and fed. If this develops into worse hypothermia (loss of gross motor skills, decreased LOC, patient stops shivering), at- tempt to warm them with hot water bottles or a hypo wrap.
Heat Exhaustion
- Not life-threatening unless it progresses to heat stroke.
- Symptoms: Mild headache, nausea, dizziness. Perhaps a slightly increased pulse and cool, clammy, skin. Rest patient in a cool place, replace lost body fluids, and eat salty foods.
Heat Stroke
- Heat stroke is much more serious than heat exhaustion.
- Symptoms: Skin is red, hot, and 50% dry and 50% wet (from sweat mechanism prioritizing vitals). Body temperature may be higher than 105 (107 is the highest survivable). The patient is disoriented, confused, combative, hallucinating; has a rapid pulse.
- Treatment: Cool the patient immediately by removing them from heat/sun and soaking them in water and fanning them (but don’t let patient shiver; this produces more heat). Hydrate them if possible. Massage limbs and evacuate them.
Dehydration
Prevention is key; keep everyone hydrated. Remember that vomiting and diarrhea can lead to dehydration.
Lightning
Don’t be the highest object. Don’t be near the highest object. Lightning flows through water, so keep your distance from lakes, ponds, etc. Remember for every 5 seconds between lightning and thunder, the storm is 1 mile away; you can be hit by lightning that is up to 3 miles away.
Consider continuing CPR past the 30 min mark if patient was the victim of a lightning strike.
Anaphylaxis
Anaphylaxis is a severe allergic reaction that can threaten the airway. The treatment is Benadryl (an anti histamine whose chemical name is diphenhydramine), which is a tablet that you swallow. If the patient’s throat is sealed because of reaction, then you must open the airway by using the EPI-PEN or Twinject which injects epinephrine into the system. Then administer Benadryl.
Note on EPI-PEN/Twinject: The autoinjector pen MUST be held in the body for 10 seconds. This is because the epinephrine drips out of the needle slowly.
Abdomen
[WFR topic. If patient has a belly ache, try to gather as much information as possible. Split abdomen into 4 parts (vertical and horizontal lines through the belly but- ton). Press on and listen (10 seconds) to each of the 4 quadrants. Examine often to see if the condition is changing. Severe abdominal pain may be passing (for example constipation) but it also may signal something extremely serious (appendicitis or ectopic pregnancy).]
Asthma
- Asthma is the narrowing of the bronchioles (respiratory tubes in chest), which leads to difficulty breathing (especially exhaling).
- Always keep an eye on any FOPpers who have asthma.
- Make sure that they are taking and necessary medication and know where they keep their inhaler.
- If a FOPper has an asthma attack, help keep them stay calm as this will help their breathing. Try matching breaths with them to bring their respiratory rate down. Let them use their inhaler if appropriate. Use EPI-PEN or Twinject as a last resort.
FOP Medkit
FOP medkits contain the following medications. Counter indication is given for all drugs. Do not administer if patient is not breathing or unable to swallow.
Ibuprofen
- Common brand name: Advil
- Appearance: Round white pills
Ibuprofen can be used to relieve pain, fever, or swelling. Each pill is 200mg; dosage for adults is one pill every 4-6 hours. If pain or fever do not respond to 1 pill, 2 pills may be used. (not to exceed 6 in a 24 hour period). Because it is anti-inflammatory (reduces swelling) it may be appropriate to use for a musculoskeletal injury involving swelling.
Side effects are rare if used properly. Abdominal or stomach cramps, pain, or discomfort (mild to moderate) ; diarrhea dizziness, drowsiness, or lightheadedness; headache (mild to moderate); heartburn, indigestion, nausea, or vomiting.
Acetaminophen
- Common brand name: Tylenol
- Appearance: individually wrapped caplets
Acetaminophen can be used to relieve minor aches, pains, headaches, and fever, but is not as effective as an anti-inflammatory. Each pill is 325 mg; standard dose for an adult is one pill every 4-6 hours. A second pill may be given if necessary, not to exceed 12 pills in a 24-hour period.
When used properly, side effects are rare. Most common is liver damage due to large does or chronic overuse.
Bismuth Subsalicylate
- Common brand name: Pepto-Bismol
- Appearance: Large round pink pills
Pepto can be used for most gastrointestinal problems, including nausea, heartburn, indigestion, upset stomach, and diarrhea (like the song). An adult dose is 2 tablets every hour as needed, not to exceed 8 doses in a 24-hour period.
Side effects are rare when used properly. But may include headache, diarrhea, drowsiness, thirst, or sweating, or dark stool.
Diphenhydramine
- Common brand name: Benadryl
- Appearance: Small oval pink pills
Diphen is an antihistamine. Anti-histamines suppress histamines, the chemicals in the body that cause allergic reactions. Anti-histamines are what can stop an allergic reaction. In the case of a severe allergic reaction, it is essential to administer anti-histamines as soon as possible, especially if the airway is in danger of closing. Dosage for adults is 1-2 (25mg) pills every 4-6 hours. In the case of a severe reaction, immediately give a double dose of antihistamine (50mg, or 2 pills).
Side effects include drowsiness; dry mouth, nose, or throat; gastrointestinal upset, stomach pain, or nausea; headache; increased appetite and weight gain; thickening of mucus.
Epinephrine (EPI-PEN or Twinject)
Epinephrine injection is used to treat life-threatening allergic reactions caused by insect bites, foods, medications, latex, and other causes. Symptoms of allergic reaction include wheezing, shortness of breath, low blood pressure, hives, itching, swelling, stomach cramps, diarrhea, and loss of bladder control. Epinephrine is in a class of medications called sympathomimetic agents. It works by relaxing the muscles in the airways and tightening the blood vessels (that is, it is a bronchodilator and a vasoconstrictor).
Side effects include upset stomach, vomiting, sweating, dizziness, nervousness, weakness, pale skin, headache, shaking hands that you cannot control. More rare and more serious symptoms are difficulty breathing, pounding, fast, or irregular heartbeat.
